I had one simple surgery to lower my risk of the deadliest cancer for women. Here’s why you probably don’t know about it—but should
I woke up from surgery groggy, with three minuscule incisions in my abdomen and huge peace of mind. I’d just had my fallopian tubes laparoscopically removed, as it’s the best—and possibly only—defense against ovarian cancer, which, though rare, is the most lethal gynecological cancer there is.
There is no detection method for ovarian cancer (a common misunderstanding is that it’s the pap smear, but that’s for cervical cancer). That’s largely because of something discovered relatively recently: About 80% of the time, cancer of the ovaries forms in the fallopian tubes, which are not easily reached or biopsied. So the cancer is not found until it spreads beyond the tubes, by which point it has typically reached a later stage and is harder to treat, with cure rates as low as 15%.
The cancer and its pre-cancer lesions are also not detectable through blood tests.
I myself had no idea about any of this until 2023, when I wrote about the Ovarian Cancer Research Alliance (OCRA) making sweeping recommendations: that all women get genetically tested to know their risk of the disease, and that all women, regardless of their risk factor, consider having what’s called an opportunistic salpingectomy—the prophylactic removal of fallopian tubes if and when they are already having another abdominal surgery.
The strategy—endorsed by the American College of Obstetrics & Gynecology since 2015—was believed to cut down the risk of ovarian cancer by up to 60%. It was adopted as a wide recommendation after a sobering U.K.-based clinical trial followed 200,000 women for more than 20 years and found that screening and symptom awareness do not save lives.
As a breast cancer survivor, the idea of ovarian cancer possibly hanging out in my fallopian tubes was haunting. So when I had the opportunity to get them removed during a recent minor abdominal surgery, I seized it.
Recovery from the anesthesia—along with incision-site soreness and uncomfortable bloating from the gas the surgeon pumped into my belly so she could see her way around—slowed me down for about a week, while waiting for the internal healing kept me out of the gym for a month. But now I feel incredibly relieved about my decision.
That’s especially true in light of major new findings out of Vancouver, British Columbia, which started a public campaign about prophylactic salpingectomy in 2010 and has been following about 80,000 people—half who opted for the procedure and half who did not—ever since. The results, announced in March 2024 at a meeting of the American Association for Cancer Research and again at a recent annual meeting of the Society of Gynecologic Oncology, were major: that salpingectomy cuts down one’s risk of ovarian cancer by a staggering 80%.
“There’s very little in medicine that gets you an 80% risk reduction,” says study lead Gillian Hanley, associate professor of obstetrics and gynecology at the University of British Columbia. “It’s remarkable.”
So why don’t more women know about it?
The effort to raise awareness of opportunistic salpingectomy
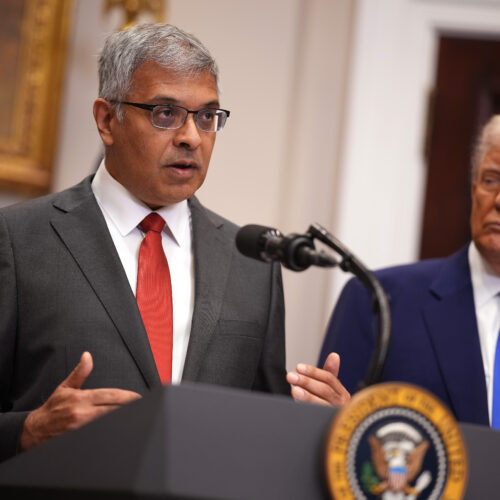
Dr. Rebecca Stone, a gynecologic oncologist at Johns Hopkins Medicine, is a leader in the effort to get the word out about preventing ovarian cancer—diagnosed in about 20,000 Americans a year and killing over 12,000. Seeing so many patients die was something that kept the surgeon awake at night.
She began to truly make opportunistic salpingectomy her mission starting in 2023, when the dismal U.K. trial results prompted organizations like OCRA to make headlines with the new recommendations.
“When all that came out, I was like, ‘Oh, great. Thank God.’ But I was also like, ‘We’re not ready yet,’” Stone tells Fortune.
That’s because there was no infrastructure around making salpingectomy the norm—no educational materials for women to leaf through while waiting at the gynecologist’s office, no awareness among non-gynecological (and even some gynecological) surgeons about offering the procedure, and not even any billing codes that would make insurance coverage for the procedure possible.
Around the same time, Stone was asked to join a meeting of the scientific advisory board for Break Through Cancer, a collaborative effort among top researchers and physicians to prevent and cure the deadliest cancers. Someone asked her if she knew how to cure ovarian cancer.
“I was like, ‘Believe me, I’ve been trying. Sometimes we get lucky, but most of the time I bury my patients,’” she says. “And then I said, ‘But we do know how to prevent it.’” At that, she recalls, “People’s hair blew back.” Not even the top cancer minds on the call had heard about the effectiveness of salpingectomy.
That call led to the creation of a new Break Through Cancer initiative, Intercepting Ovarian Cancer, which aims to both improve detection of fallopian tube pre-cancers and to expand salpingectomy as a prevention tool within the general population. Stone has already succeeded in working with the Centers for Disease Control and Prevention to create specific billing codes for the procedure, and is now gearing up to launch the Outsmart Ovarian Cancer Campaign with Memorial Sloan Kettering gynecologic surgeon Dr. Kara Long.

“Remember when smoking cessation was a cancer prevention strategy that people got behind? The billboards and advertisements? That is, I think, what we need here,” says cancer biologist Tyler Jacks, Break Through Cancer’s president.
“This is a systemic problem that will take true cultural change within the medical community and beyond to solve,” adds OCRA president and CEO Audra Moran about the slow adoption of salpingectomy. “We know it’s not being adopted as widely as it could be.”
Indeed, there are still barriers to the effort—including how to present the issue with sensitivity in some communities of color, which carry the historic U.S. burden of coercive sterilization; convincing some surgeons that there is enough evidence behind it, as all of it up until the Vancouver findings has been based on historic data; and also the idea of surgical prevention itself, which can be off-putting.
But there is another surgical prevention embraced as the norm, Stone is quick to point out. “It’s called a colonoscopy,” she says, “And the risks of the colonoscopy are much higher,” including the possibility of bowel perforation. “And then, guess what? You have to do it all again in five or 10 years.” Salpingectomy, she argues, is a one-and-done, and is “much more cost-saving” in the long run.
Plus, notes Hanley, “of course, we are not suggesting that every person with fallopian tubes needs to go and have them surgically removed. That will never be the recommendation. It is a surgical intervention, and surgery is not without risk.” But she does see the approach as “exciting,” as, “for so many years, we have not had a lot of cancer prevention that was not lifestyle-focused—revolving around diet, exercise, environmental exposure to carcinogens, and things that are really challenging to change.”
Is salpingectomy right for you?
Anyone finished having children or not planning on having children who is already going to have another abdominal surgery—appendectomy, gallbladder removal, hysterectomy, for example—is a candidate for opportunistic salpingectomy.
“What we’re really saying is that if you are already having some kind of a surgery, because of some other benign disease that you’re treating, and the surgeon is there already, we have really compelling evidence that adding this to another procedure does not change your risks at all compared to what you would already risk with surgery,” Hanley says.
If you’re not having another surgery and really want your fallopian tubes removed anyway, you could opt to do it as a route to sterilization (instead of tubal ligation), which it technically is.
Women at high risk—such as the less than 1% who have a genetic mutation such as BRCA1 or BRCA2, which raises the risk of ovarian cancer from 1% to 5%—“should be recommended a stand-alone salpingectomy for risk reduction,” says Stone. They might also consider an oophorectomy—removal of the ovaries—depending on their age, she adds.
While the long-term risks of salpingectomy, if any, are not known, there are no short-term risks, as fallopian tubes don’t serve any known purpose beyond reproduction—as opposed to the ovaries, which still produce important hormones likely well beyond menopause, she says.
I opted to keep my ovaries. But these decisions are, of course, highly personal. I never thought I’d be someone to get elective surgery in the first place, but the statistics convinced me.
As for Stone, she says she has spent too many hours in the operating room trying to save patients “with this horrible disease” to give up on awareness.
“I am going to spend every minute of my remaining life to get this information out there,” she says, “and to reach as many people as humanly possible.”
More on women and cancer:
- 3 in 4 women are skipping a routine appointment and putting themselves at higher risk for cancer
- With ovarian cancer, there’s no such thing as early detection. Here’s what to learn from tennis great Chris Evert’s battle with the disease
- Women will now be notified about breast density after mammograms. Here’s what should happen next
This story was originally featured on Fortune.com


© Getty Images